ABOUT YOUR INGUINAL HERNIA AND LAPAROSCOPIC REPAIR:
Approximately 600,000 inguinal or groin hernia repair operations are performed annually in the United States. Some are performed by the conventional “open” method. Some hernia repairs are performed using a small telescope known as a laparoscope. If your surgeon has recommended a hernia repair, this brochure can help you understand what a hernia is and what your treatment options are.
About Hernias
WHAT IS A HERNIA?
- A hernia is a gap or space in the strong tissue that holds muscles in place. A hernia occurs when the inside layers of the abdominal muscle have weakened, resulting in a bulge or tear. In the same way that an inner tube pushes through a damaged tire, the inner lining of the abdomen pushes through the weakened area of the abdominal wall to form a small balloon like sac. This can allow a loop of intestine or abdominal tissue to push into the sac. The hernia can cause discomfort, severe pain, or other potentially serious problems that could require emergency surgery.
- Both men and women can get a hernia.
- You may be born with a hernia (congenital) or develop one over time.
- A hernia does not get better over time, nor will it go away by itself. There are no exercises or physical therapy regimen that can make a hernia go away.
HOW DO I KNOW IF I HAVE AN INGUINAL HERNIA?
- The common areas where hernias occur are in the groin (inguinal), belly button (umbilical), and the site of a previous operation (incisional).
- It is usually easy to recognize a hernia. You may notice a bulge under the skin. You may feel pain or discomfort when you lift heavy objects, cough, strain during urination or bowel movements, or during prolonged standing or sitting. Other times a hernia may be detected by your doctor on a routine physical examination.
- The pain may be sharp and immediate or a dull ache that gets worse toward the end of the day.
- Severe, continuous pain, redness, and tenderness are signs that the hernia may be entrapped or strangulated. Another sign of this is if the bulge used to come and go, but now is stuck out. These symptoms are cause for concern and you should immediately contact your physician or surgeon.
WHAT CAUSES AN INGUINAL HERNIA?
The wall of the abdomen has natural areas of potential weakness. Hernias can develop at these or other areas due to heavy strain on the abdominal wall, aging, injury, an old incision or a weakness present from birth. Anyone can develop a hernia at any age. Most hernias in children are congenital. In adults, a natural weakness or strain from heavy lifting, persistent coughing, difficulty with bowel movements or urination can cause the abdominal wall to weaken or separate.
WHAT ARE THE ADVANTAGES OF LAPAROSCOPIC INGUINAL HERNIA REPAIR?
Laparoscopic Hernia Repair is a technique to fix tears in the abdominal wall (muscle) using small incisions, telescopes and a patch (mesh). Laparoscopic repair offers a shorter return to work and normal activity for most patients.
ARE YOU A CANDIDATE FOR LAPAROSCOPIC INGUINAL HERNIA REPAIR?
Only after a thorough examination can your surgeon determine whether laparoscopic hernia repair is right for you. The procedure may not be best for some patients who have had previous abdominal surgery, prostate surgery, or underlying medical conditions.
Laparoscopic Inguinal Hernia Repair
WHAT PREPARATION IS REQUIRED?
- Most hernia operations are performed on an outpatient basis, and therefore you will probably go home on the same day that the operation is performed.
- Preoperative preparation includes blood work, medical evaluation, and an EKG depending on your age and medical condition.
- After your surgeon reviews with you the potential risks and benefits of the operation, you will need to provide written consent for surgery.
- It is recommended that you shower the night before or morning of the operation with an antibiotic soap.
- After midnight the night before the operation, you should not eat or drink anything except medications that your surgeon has told you are permissible to take with a sip of water the morning of surgery.
- Drugs such as aspirin, blood thinners, anti-inflammatory medications (arthritis medications) and Vitamin E may need to be stopped temporarily for several days to a week prior to surgery. Your surgeon will discuss this with you and provide instructions regarding your medications around the time of surgery.
- Diet medication or St. John’s Wort should not be used for the two weeks prior to surgery.
- Quit smoking and arrange for any help you may need at home. Smoking may increase the risk of the hernia recurring, or coming back after surgery. In some cases, your surgeon may require that you quit smoking prior to surgery.
HOW IS THE PROCEDURE PERFORMED?
There are few options available for a patient who has a hernia.
- Use of a truss (hernia belt) is rarely prescribed as it is usually ineffective. It may alleviate some discomfort, but will not prevent the possibility of bowel incarceration or strangulation.
- Most hernias require a surgical procedure.
- Surgical procedures are done in one of two fashions:
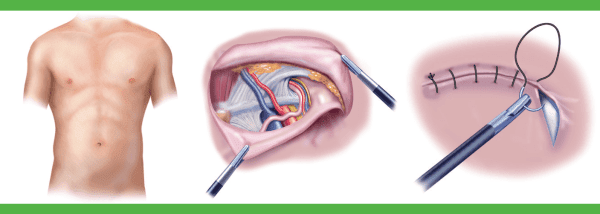
- The open approach is done from the outside through a three to four inch incision in the groin or the area of the hernia. The incision will extend through the skin, subcutaneous fat, and allow the surgeon to get to the level of the defect. The surgeon may choose to use a small piece of surgical mesh to repair the defect or hole. This technique can be done with a local anesthetic and sedation, using a spinal anesthetic or a general anesthetic.
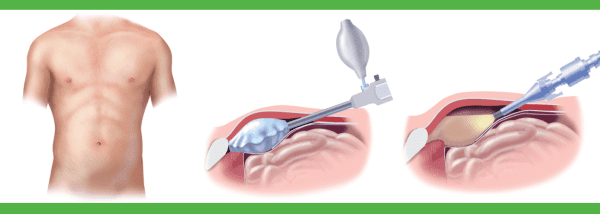
- The laparoscopic hernia repair is done with the use of a laparoscope (a tiny telescope) connected to a special camera is inserted through a cannula, a small hollow tube, allowing the surgeon to view the hernia and surrounding tissue on a video screen.
Other cannulas are inserted which allow your surgeon to work “inside.” Three separate quarter inch incisions are usually necessary. The hernia is repaired from behind the abdominal wall. A small piece of surgical mesh is placed over the hernia defect, and it may be fixed in place using staples, adhesive sealant, or sutures. This operation is usually performed with general anesthesia.
WHAT HAPPENS IF THE OPERATION CANNOT BE PERFORMED OR COMPLETED BY THE LAPAROSCOPIC METHOD?
In a small number of patients the laparoscopic method cannot be performed. Factors that may increase the possibility of choosing or converting to the “open” procedure may include obesity, a history of prior abdominal surgery causing dense scar tissue, inability to visualize organs or bleeding problems during the operation.
The decision to perform the open procedure is a judgment decision made by your surgeon either before or during the actual operation. When the surgeon feels that it is safest to convert the laparoscopic procedure to an open one, this is not a complication, but rather good surgical judgment. The decision to convert to an open procedure is strictly based on patient safety.
After Surgery
WHAT SHOULD I EXPECT AFTER SURGERY?
- Following the operation, you will be transferred to the recovery room where you will be monitored for 1-2 hours until you are fully awake.
- Once you are awake and able to walk, drink liquids, and urinate, you will be sent home.
- With any hernia operation, you can expect some soreness mostly during the first 24 to 48 hours.
- You are encouraged to be up and about the day after surgery.
- With laparoscopic hernia repair, you will probably be able to get back to your normal activities within a week. These activities include showering, driving, walking up stairs, lifting, working and engaging in sexual intercourse.
- Call and schedule a follow-up appointment within 2 weeks after you operation.
Complications
WHAT COMPLICATIONS CAN OCCUR?
- Any operation may be associated with complications. The primary complications of any operation are bleeding and infection, which are uncommon with laparoscopic hernia repair.
- There is a very low risk of injury to the urinary bladder, the intestines, blood vessels, nerves or the sperm tube going to the testicle.
- Difficulty urinating after surgery can occur and may require placement of a catheter, or tube to drain the bladder after surgery. You should ask your surgeon about ways to prevent this from occurring before your operation.
- Bruising and swelling of the scrotum, the base of the penis, and the testicles is not uncommon with open and laparoscopic repair. This will gradually resolve on its own in the vast majority of patients.
- Any time a hernia is repaired it can come back. This long-term recurrence rate is low in patients who undergo laparoscopic repair by an experienced surgeon. Your surgeon will help you decide if the risks of laparoscopic hernia repair are less than the risks of leaving the condition untreated.
- It is important to remember that before undergoing any type of surgery–whether laparoscopic or open–you should ask your surgeon about his/her training and experience with the operation.
WHEN TO CALL YOUR DOCTOR
Be sure to call your physician or surgeon if you develop any of the following:
- Persistent fever over 101 degrees F (39 C)
- Bleeding
- Increasing abdominal or groin swelling
- Pain that is not relieved by your medications
- Persistent nausea or vomiting
- Inability to urinate
- Chills
- Persistent cough or shortness of breath
- Foul smelling drainage (pus) from any incision
- Redness surrounding any of your incisions that is worsening or getting bigger
- You are unable to eat or drink liquids
This information is not intended to take the place of your discussion with your surgeon about the need for laparoscopic inguinal hernia surgery. If you have questions about your need for hernia surgery, your alternatives, billing or insurance coverage, or your surgeons training and experience, do not hesitate to ask your surgeon or his/her office staff about it. If you have questions about the operation or subsequent follow-up, please discuss them with your surgeon before or after the operation.